In early 2020 (how long ago that feels) we were told that lockdown would ‘send the coronavirus packing’. Exaggerated claims were also made on behalf of a ‘world beating’ test and trace system which similarly failed to live up to expectations. Next it was the turn of vaccination – the magic bullet that would put an end to the crisis once and for all. Except…. that in November a new variant, Omicron, appeared on the scene, swept the board and changed the landscape once again. As the new year began, there were 218,724 positive test results reported in the UK in one day.
Nonetheless, Health Secretary Sajid Javid, is proud that we have the least protective measures in place in Europe. He insists ‘we must give ourselves the best chance of living alongside the virus’. The prime minister’s message in the lead up to New Year was ‘celebrate New Year’s Eve but exercise caution and take tests’. Once again the public health message was unclear. To this problem of ambiguity (what does ‘exercise caution’ mean?) was added a wide unavailability of lateral flow tests (LFTs) as well as a misrepresentation of what they can and cannot do.
Lateral flow tests
Shortage of LFTs was related both to advice to the public that they test frequently before social contact and to the increase in demand through rising case numbers. Hospital staff (who are asked to test twice weekly) were finding it difficult to find tests. As it turned out, Alliance Healthcare, the sole distributor of LFT to pharmacies closed for four days over Christmas just as it received a delivery of 2.5m devices.
The prime minister has previously wrongly stated that LFTs ‘identify people who are infectious … allowing those who are not infectious to continue as normal’. The reality is less clear cut. Studies show that even when the test is done by expert nurses, virus is detected only in 73% of cases, falling to 58% when performed by testing centre employees. It is likely that reliability is even lower in tests performed by members of the public. Preliminary testing in Liverpool of mostly asymptomatic people showed that LFTs only detected 50% of those with a positive PCR (the gold standard for testing), while 30% of those with high viral loads were missed. As the manufacturer Innova advises ‘Negative results do not rule out SARS-CoV-2 infection and should not be used as the sole basis for treatment or patient management decisions, including infection control decisions.’ This is endorsed by the World Health Organization that says negative antigen rapid diagnostic test results ‘should not remove a contact from quarantine requirements.’ Giving people the ‘all clear’ on the basis of a negative LFT is likely to have contributed to the spread of infection, adding to the damage already done by the private laboratory which issued 43,000 false negative tests.
The NHS is now on a ‘war footing’. However, as case numbers increase, plans have been announced not to introduce measures aimed at reducing spread of infection, but to build eight ‘Nightingale hubs’ – these latter to provide additional surge capacity for patients in unused space or car parks of hospitals. Like the original Nightingale Hospitals, it is unclear how these might be staffed. There can be no doubt, however, that the NHS is severely stretched with a reduced number of 90,000 adult acute beds running at 90% capacity and lack of social care already preventing many from being discharged from hospital.
Critical voices
Chris Whitty, Chief Medical Officer for England, said of Omicron: ‘This is a really serious threat at the moment. How big a threat? There are several things we don’t know, but all the things that we do know, are bad….and the principle one being the speed at which this is moving, it is moving at an absolutely phenomenal pace.’ Case numbers were in fact doubling in little over two days. Even though there was some suggestion that the disease caused is not as severe as with the Delta variant, the very large numbers of cases risked affecting many areas of the economy and overwhelming the health service. The government, however, decided to continue with a ‘cross your fingers and hope for the best’ approach, relying wholly on booster vaccination as a way of dealing with this new threat.
Members of Independent SAGE, likened the government’s stance to playing Russian roulette. The Independent SAGE advised before Christmas that spread of infection must urgently be reduced by closing indoor hospitality and entertainment; no indoor gatherings held between households; all close contacts of new cases should isolate for 10 days and be given appropriate support (e.g. the two million people not entitled to sick pay). They argued that the overall focus should be on decreasing cases to as low a level as possible in order to prevent disruption to key services and prevent demands on an already stretched NHS outstripping available resources. Increased restrictions in other countries such as the Netherlands were effectively driving down cases. A precautionary approach was justified given the very rapid rise in cases coupled with uncertainty about the overall impact of Omicron. Their warning went unheeded but has proved prophetic.
Reducing viral transmission
A key focus should also be to make the environment safer through air filtration and effective ventilation. This should also be a priority not just in workplaces, but also for schools. The impact of covid-19 in terms of physical illness in children is often played down. But by the start of December, 37 children under 15 years of age had died from covid in the UK together with a further 41 15-19 y olds. Six thousand 6-17 y olds had been hospitalised and 77,000 infected children were reported to have prolonged symptoms of fatigue and cognitive dysfunction. Over 1 million children <16 y have been infected since last September. Current surveys indicate that almost 6% of under 12s are infected, and over 3% of primary school children as of the end of December.
There is an argument for vaccinating all 5-11 year olds to prevent spread of infection, and US experience indicates this is safe. Although this has not yet been approved by the Joint Committee on Vaccination and Immunisation. Other needed interventions for schools include reintroduction of face masks (now grudgingly conceded for secondary school pupils); isolation of household contacts until a negative PCR test obtained; reinstatement of bubbles/cohorts; onsite testing – perhaps with saliva samples to monitor for outbreaks; staggering school start times.
It is disappointing that the government see little urgency in any of these measures. While 300,000 carbon dioxide monitors have been sent out to schools to help monitor air quality, distribution has been chaotic and numbers of devices amount to only two per school rather than one for every classroom. Staff also need guidance on how to best use them, since they only monitor air exchange and don’t provide clean air. Filtration units (with High Efficiency Particulate-Absorbing filters) are effective in reducing viral aerosols, but should be paid for by government rather than taken out of existing school budgets as required currently. It has been estimated that the cost for this would be half the money being spent on the recently commissioned Royal Yacht. Insisting on the right to clean air at work as a way of reducing the spread of infection must be a key demand for trade unions and health and safety workplace representatives to take up.
Consequences of current government strategy
Defenders of the current UK public health approach justify their support by pointing out that hospitals have not yet filled up with very sick patients (although of course, if that does happen it will be too late). Claiming not so many people become seriously ill as with the Delta variant is premature. In the US, the respected infectious disease authority Dr Anthony Fauci pointed out that while there is evidence Omicron might be associated with less severe disease, caution was still needed as such high transmission rates could still lead to unmanageable demand for health care.
We have still to find out what the effect of Christmas and New Year mixing will be, although meanwhile there are very real adverse consequences for many. Already in the UK by the end of December, numbers of hospital inpatients with covid had increased to nearly 10,000, up 38% from the previous week (but so far nowhere near as the peak of 34,000 patients one year ago). Numbers dying from covid-19 are currently averaging around 112/day (a staggering one every 13 minutes), somewhat down on figures for November with its peak of 1,176 deaths in one week.
Some seek to minimise the scale of the problem by pointing out that in around 20% of hospital patients with positive covid tests, this is an incidental finding and has not “caused the admission”. This is impossible to tell. Moreover, acquiring covid often makes an underlying chronic condition worse, for example in patients with diabetes or inflammatory bowel disease, and so may precipitate an admission – even if covid is not being the main reason for admission. These patients still add to the overall burden on the NHS and their number should not be disregarded.
Not everyone is vaccinated or can be easily protected
In addition to vulnerable patients (those with chronic medical conditions, including the immuno-suppressed), there are still large numbers of people unprotected. Around 5 million people eligible for vaccination have not been immunised with the unvaccinated accounting for around 60% of London ICU patients. Vaccine uptake is variable, higher in more affluent areas and only around 50% in some deprived areas. For children over 12 years, 90% have had at least one dose, 82% two doses and 56.5% two doses and booster. Immediately before Christmas, 1 in 25 people in England were infected (rising to 1 in 6 20 year olds in London). This emphasises the need for reducing viral spread rather than focusing entirely on the vaccination programme.
Wider impact of surge in cases
Staff absences through illness or need to isolate are badly affecting hospitals, community services and care homes. NHS staff absences totalled 24,632 in acute trusts because sick or quarantining at the end of December; this was double the figure from two weeks earlier. There was a total of 68,000 staff off sick from all causes (many through stress) on 26th December. The British Medical Association has called for cancellation of large social gatherings and limits on social mixing. It has also demanded that staff have access to protective face masks, since, astonishingly, this is still not routine.
The Government appears to base its decision making only on hospital statistics without giving due consideration to the impact on GP and community services and wider society, even though this is considerable. Multiple NHS trusts across England have now declared ‘critical incidents’ (i.e. concerns about no longer being able to offer safe care to patients) amid soaring staff absences, with health leaders saying many parts of the services are in a state of crisis. In Manchester alone, 17 hospitals have paused non-urgent surgery and appointments.
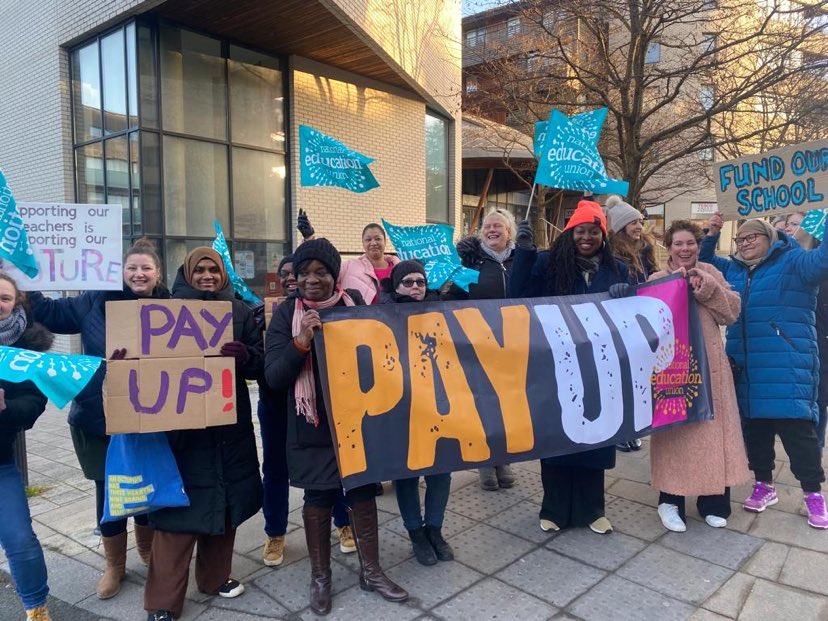
Covid is also having a major effect on other frontline services with 15% of London fire service staff off work on the 27th December. School leaders in England are warning of weeks of disruption owing to high levels of staff covid absences, which could lead to children being sent home to learn remotely. Dr Mary Bousted, the joint general secretary of the National Education Union, said it was ‘alarming’ that the education secretary, Nadhim Zahawi, was advocating the infection spreading strategy of combining classes to overcome staff shortages.
Rubbish bins across parts of England are overflowing with household detritus from the Christmas period where collections have been cut back because of staff sickness. Ambulance trusts have begun asking patients with heart attacks and strokes to get a lift to hospital with family or friends instead of waiting for an ambulance, because of high covid absences and ‘unprecedented’ surges in demand. UK train operators have cut hundreds of services due to staff sickness.
Conclusions
The current policy of relying solely on vaccine roll out while letting case numbers skyrocket is very high risk. Further chaos in education is likely to add to the already considerable impact of the pandemic on children. The NHS is buckling under the strain, and even if optimistic predictions of the impact of Omicron in terms of hospital admissions and death prove true, staff are suffering extreme stress trying to keep the system going. Meanwhile many patients with non-covid illness are getting sub-standard care and joining ever lengthening waiting lists.
One commentator with close links to many working in health care spoke in disbelief that: ‘Ministers telling us there is nothing in the data that indicates further measures are required is feckless, stupid, criminal, mendacious-blindness.’
A clearly frustrated Matthew Taylor, chief executive of the NHS confederation, made a heartfelt plea:
‘over the coming days, instead of making optimism and complacency a kind of political virility symbol let’s focus on facts, let’s wait for the data, let’s listen to those trying to cope on the frontline. Most of all, instead of turning the science and policy on COVID-19 into a new terrain for the culture wars, let’s try to get through these next few weeks together.’
Prime minister Johnson, (perhaps modelling himself more on Nero rather than Churchill) predicted that we will ‘ride out this Omicron wave’.
One important question is why the Westminster government is going down this dangerous road? This no doubt is partly due to the internal political differences within the Conservative party, with the Right-wing of the party now holding the prime minister hostage. In addition, we are not all equal in the face of covid, with those like our political class, least affected by social and economic inequalities being least at risk of death. Could it be that the elderly, the poor and the disabled are simply seen as expendable? It is also probable that with an eye to the next election, the government is desperate to protect an already damaged economy and hopes any success here will ultimately deflect from its appalling handling of the pandemic. If the hope is that by avoiding restrictions economic activity will continue unabated, outstripping our European rivals, the prime minister should be made aware that the evidence strongly suggests containing covid versus saving the economy is a false dichotomy. Optimism and complacency will not serve the public well and are likely to cost many more lives in the coming months.
A global ‘vaccine-plus’ response is needed
Coronavirus is a global pandemic and can only be approached on a global scale. Worldwide, only 8.4% of people in low income countries have had at least one dose of vaccine. Poor international planning, vaccine ‘dumping’ by the richer countries of out-dated stocks, in the face of the difficult logistics of keeping vaccine at low temperature during distribution has meant that supplies from COVAX to Nigeria had to be destroyed. The World Health Organization is aiming for 70% of the world’s population to be vaccinated by June 2022. This would need not just the waiver of intellectual property rights by the manufacturers (something blocked by the UK government) but also technology transfer and building expertise to enable local production. For this a global funding mechanism would need to be in place so that vaccine availability could be guaranteed when planning roll out. Without this, there seems every likelihood that further variants will arise and spread rapidly around the globe. Clearly provision of vaccine to lower and middle income countries should be a priority for rich countries, working together with the WHO. Until that happens, we should not be surprised by new variants and should agree in advance on how to respond and what the trigger would be.
It is time for a vaccine-plus approach to be adopted globally (including the UK), based not only on vaccine equity, but also prevention of viral transmission. Advocates suggest that this strategy will slow the emergence of new variants and ensure they exist on a low transmission background where they can be controlled by effective public health measures, while allowing everyone (including those clinically vulnerable) to go about their lives more freely.
John Puntis is the co-chair of Keep Our NHS Public